Pulmonary embolism (PE), a serious condition where blood clots block arteries in the lungs, is often associated with respiratory and cardiovascular complications. However, the neurological consequences of PE, including the potential for a clot to travel to the brain, are less widely understood. This article explores the connection between venous thromboembolism (VTE), which encompasses both deep vein thrombosis (DVT) and PE, and neurological complications, with a focus on whether a pulmonary embolism can travel to the brain and the potential risks involved.
Understanding Venous Thromboembolism (VTE) and Pulmonary Embolism (PE)
Venous thromboembolism (VTE) is a condition where blood clots form in the veins, most commonly in the legs (DVT). These clots can then travel through the bloodstream and lodge in the pulmonary arteries, causing a pulmonary embolism (PE). While VTE is often underdiagnosed, it’s a significant cause of cardiovascular mortality. Key factors contributing to VTE include venous stasis, hypercoagulability, and endothelial injury, known as Virchow’s triad.
Neurological Complications Following VTE: An Overview
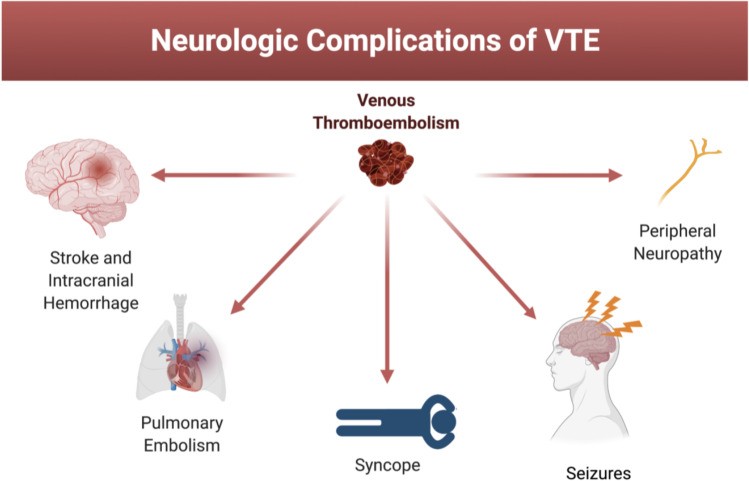
While VTE is well-known as a complication of neurological diseases, the reverse – neurological complications following VTE – is less studied. These complications can be categorized into:
- Central Nervous System (CNS) Complications: Intracranial hemorrhage and ischemic stroke.
- Atypical Presentations of PE: Syncope and Seizures
- Peripheral Nervous System (PNS) Complications: Peripheral neuropathy and neuropathic pain syndromes
The Link Between Pulmonary Embolism and Stroke
The most concerning aspect of a PE traveling to the brain is the potential to cause a stroke. There are two primary ways in which VTE can lead to stroke:
- Intracranial Hemorrhage (ICH): Anticoagulants and thrombolytics, used to treat VTE, can increase the risk of bleeding in the brain, leading to ICH.
- Ischemic Stroke: While less common, VTE can contribute to arterial events like ischemic stroke. Studies have shown an increased risk of ischemic stroke in patients with DVT and PE.
Patent Foramen Ovale (PFO): A Pathway for Paradoxical Embolism
A patent foramen ovale (PFO) is a persistent opening between the right and left atria of the heart. In the general population the prevalence of PFO is about 25%. However, it’s much higher, about 50%, in younger people less than 55 years old that have cryptogenic strokes. This condition, present in a significant portion of the population, can create a pathway for paradoxical embolism, where blood clots from the venous system bypass the lungs and travel directly to the arterial system, potentially reaching the brain. In patients with a PFO, a PE can lead to a stroke if the clot passes through the PFO and into the brain’s blood supply.
 Patent Foramen Ovale and Neurological Complications of VTE
Patent Foramen Ovale and Neurological Complications of VTE
Alt text: Illustration showing the link between venous thromboembolism (VTE) and neurological complications, including intracranial hemorrhage, ischemic stroke, syncope, seizures and peripheral nervous system complications.
Risk Factors and Diagnosis
Several factors can increase the risk of stroke in individuals with VTE:
- Presence of PFO: As discussed above, PFO provides a direct route for clots to bypass the lungs.
- May-Thurner Syndrome (MTS): This condition, where the right iliac artery compresses the left iliac vein, increases the risk of left leg DVT, potentially leading to PE and stroke.
- COVID-19 Infection: SARs-CoV-2 has been associated with blood clots, including MI, VTE, and ischemic stroke
- Malignancies: Increased incidence of VTE associated with malignancy
Diagnosis of PFO typically involves echocardiography, either transthoracic (TTE) or transesophageal (TEE), with agitated saline contrast to detect the passage of bubbles through the opening. In patients with PE and confirmed PFO, a higher suspicion for silent ischemic events is warranted, and diffusion-weighted brain MRI may be used to detect these events.
Atypical Presentations: Syncope and Seizures
Besides the more common CNS and PNS complications of VTE, syncope and seizures can also be atypical neurologic presentations of PE.
- Syncope: Can be caused by RV failure, arrhythmias or a vasovagal reflex.
- Seizures: Transient global cerebral hypoperfusion, or hypoxia-driven cardiogenic seizures.
Peripheral Nervous System Complications of VTE
VTE, and its treatment, can affect the PNS, commonly causing post-thrombotic syndrome (PTS). PTS can cause neuropathic pain due to inflammation surrounding affected nerves, direct entrapment neuropathy from DVT or VTE treatment.
Prevention and Management
Preventive measures include:
- Anticoagulation: Medications like DOACs, VKAs, or LMWH can prevent further clot formation and reduce the risk of stroke.
- PFO Closure: In select patients with PFO and cryptogenic stroke, device closure of the PFO may be more effective than medical therapy alone.
- Compression Stockings: Elastic compression stockings can help prevent post-thrombotic syndrome (PTS) after DVT.
Conclusion
While the primary concern with pulmonary embolism is its impact on the lungs and heart, the potential for neurological complications, including stroke, cannot be ignored. A clot can travel to the brain, especially in individuals with underlying conditions like PFO. Vigilant monitoring, prompt diagnosis, and appropriate management strategies are essential to minimize the risk of these potentially devastating neurological sequelae. Further research is needed to better understand the complex relationship between VTE and neurologic complications, ultimately improving patient outcomes.
