Are you wondering, “Can You Travel After Angiogram?” Yes, generally, air travel is possible a couple of days after an angiogram or angioplasty. TRAVELS.EDU.VN emphasizes that individual circumstances vary, and consulting your doctor before planning any trips is crucial. This guide provides comprehensive information on post-angiogram travel, focusing on safety, precautions, and expert recommendations to ensure a smooth journey, covering everything from cardiac rehabilitation support to understanding post-procedure complications and anticoagulant medication.
1. Understanding Angiograms and Their Impact on Travel
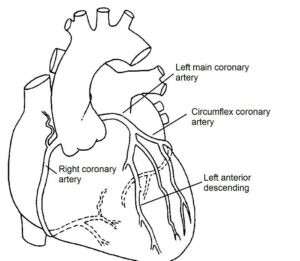
What is an angiogram, and how does it affect your travel plans? An angiogram is a diagnostic procedure that involves injecting a contrast dye into your blood vessels to visualize them using X-rays. It’s commonly used to detect blockages or narrowing in the arteries, especially those supplying blood to your heart. Understanding the procedure and its potential impact on your body is the first step in planning safe post-angiogram travel.
1.1. What is an Angiogram?
An angiogram is a minimally invasive medical procedure used to examine blood vessels. A catheter is inserted into an artery, usually in the groin or wrist, and guided to the area of interest. Contrast dye is injected to make the blood vessels visible on X-ray images. This helps doctors identify any blockages, narrowing, or abnormalities in the arteries.
1.2. Why is it Performed?
Angiograms are performed for various reasons, including:
- Diagnosing Heart Conditions: Identifying coronary artery disease, which can cause chest pain (angina) and heart attacks.
- Evaluating Blood Vessel Problems: Detecting aneurysms, blood clots, or other vascular issues.
- Planning Treatments: Guiding procedures like angioplasty or surgery.
1.3. How Does it Affect Your Body?
An angiogram can have temporary effects on your body, such as:
- Bruising and Discomfort: At the catheter insertion site.
- Reactions to Contrast Dye: Allergic reactions, although rare, can occur.
- Risk of Bleeding or Infection: At the insertion site.
- Temporary Kidney Issues: The contrast dye can sometimes affect kidney function, especially in individuals with pre-existing kidney problems.
1.4. Key Considerations for Travel
After an angiogram, several factors need consideration before traveling:
- Recovery Time: Allowing sufficient time for the insertion site to heal and for any potential complications to arise.
- Medications: Ensuring you have an adequate supply of prescribed medications and understanding their potential side effects.
- Follow-Up Appointments: Scheduling any necessary follow-up appointments to monitor your condition.
- Insurance: Checking your travel insurance policy to ensure it covers any potential medical issues related to your procedure.
2. Immediate Post-Angiogram Recovery: What to Expect
What is the immediate recovery process after an angiogram, and what precautions should you take? The first few days after an angiogram are crucial for recovery. You’ll need to monitor the insertion site for any signs of infection or bleeding and follow your doctor’s instructions regarding activity levels. This period is vital to ensure you’re in stable condition before considering travel.
2.1. Initial Monitoring
Immediately after the angiogram, healthcare professionals will monitor you closely. Key aspects of this monitoring include:
- Vital Signs: Regular checks of blood pressure, heart rate, and oxygen saturation to ensure stability.
- Insertion Site: Frequent assessment of the puncture site for bleeding, swelling, or hematoma formation.
- Pain Management: Administration of pain relief medication, if needed, to manage any discomfort at the insertion site.
2.2. Bed Rest and Limited Activity
Following the procedure, bed rest is typically required for a specific period, which can vary depending on the access site:
- Femoral Access (Groin): Patients may need to lie flat for several hours to prevent bleeding.
- Radial Access (Wrist): Bed rest may be shorter, but movement of the arm is restricted.
Limited activity is generally recommended for the first 24-48 hours, avoiding strenuous activities that could strain the insertion site.
2.3. Wound Care at Home
Proper wound care is essential to prevent complications:
- Keep the Area Clean and Dry: Gently clean the site with mild soap and water, and pat it dry.
- Monitor for Signs of Infection: Watch for increased pain, redness, swelling, pus, or fever, and report any concerns to your healthcare provider.
- Avoid Soaking: Refrain from taking baths or swimming until the site is fully healed.
2.4. Managing Discomfort
Some discomfort is normal after an angiogram, and can be managed with:
- Over-the-Counter Pain Relievers: Acetaminophen or ibuprofen can help alleviate pain.
- Ice Packs: Applying ice packs to the insertion site can reduce swelling and pain.
- Proper Hydration: Drinking plenty of fluids helps flush out the contrast dye and supports kidney function.
2.5. Medication Management
Adhering to prescribed medications is critical:
- Antiplatelet Medications: Medications like aspirin or clopidogrel may be prescribed to prevent blood clots, especially after angioplasty.
- Other Medications: Continue taking any other prescribed medications as directed by your healthcare provider.
2.6. Follow-Up Appointments
Scheduling and attending follow-up appointments are important for monitoring your recovery and addressing any potential issues. These appointments allow healthcare professionals to:
- Assess Wound Healing: Ensure the insertion site is healing properly.
- Monitor Kidney Function: Check kidney function, especially if you have pre-existing kidney problems.
- Adjust Medications: Make any necessary adjustments to your medication regimen.
 Person resting after angiogram
Person resting after angiogram
3. Flying After Angiogram: Safety and Recommendations
How soon can you fly after an angiogram, and what precautions should you take during air travel? The general guidance is that flying is typically safe after two days following an angiogram or routine angioplasty, according to the UK Civil Aviation Authority. However, individual circumstances can vary, and it’s essential to consult with your doctor. Factors such as the complexity of the procedure, your overall health, and potential complications influence the recommendation.
3.1. General Guidelines for Flying
The UK Civil Aviation Authority provides general guidelines regarding fitness to fly:
- After Angiogram or Routine Angioplasty: You may be able to fly after 2 days.
- After Uncomplicated Heart Attack: You may be able to fly after 3 – 10 days.
- After Significant or Complicated Heart Attack: Delay flying for 4 – 6 weeks.
3.2. Consulting Your Doctor
It is crucial to discuss your individual circumstances with your doctor or nurse before planning air travel. They can assess your specific situation and provide personalized recommendations based on factors such as:
- Type of Procedure: Whether you had an angiogram alone or an angioplasty with stent placement.
- Overall Health: Your general health status and any other medical conditions you have.
- Potential Complications: Whether you experienced any complications during or after the procedure.
3.3. Essential Precautions During Air Travel
To ensure a safe and comfortable flight after an angiogram, consider the following precautions:
- Stay Hydrated: Drink plenty of water to prevent dehydration, which can increase the risk of blood clots.
- Move Around: Get up and walk around the cabin every hour to promote blood circulation.
- Wear Compression Stockings: Compression stockings can help prevent blood clots in your legs.
- Avoid Alcohol and Caffeine: These substances can dehydrate you and affect your heart rhythm.
- Manage Stress: Practice relaxation techniques to minimize stress, which can strain your heart.
- Carry Medications: Keep all your medications in your carry-on luggage and ensure they are clearly labeled.
3.4. Potential Risks and Complications
While flying is generally safe after an angiogram, be aware of potential risks and complications:
- Deep Vein Thrombosis (DVT): Prolonged immobility during flights can increase the risk of blood clots in the legs.
- Changes in Air Pressure: Changes in cabin pressure can affect your heart and blood vessels.
- Limited Medical Assistance: Access to medical care may be limited during a flight.
3.5. Medical Insurance Considerations
Before traveling outside the UK, ensure you have adequate medical insurance. Inform your insurance company of your heart condition and be aware that many medical insurance companies may not provide coverage within 1 month of an angioplasty procedure.
4. Driving After Angiogram: Rules and Safety Tips
What are the driving restrictions after an angiogram, and how can you ensure your safety on the road? According to the DVLA (Driver and Vehicle Licensing Agency), specific guidelines exist for driving after an angiogram or angioplasty. Generally, you should not drive for three days after an angiogram and one week after a planned angioplasty. If you have had a heart attack, the return to driving depends on how well the heart muscle is pumping.
4.1. DVLA Recommendations
The DVLA provides the following recommendations regarding driving after cardiac procedures:
- After an Angiogram: Do not drive for 3 days.
- After a Planned Angioplasty: Do not drive for 1 week.
- After a Heart Attack: Return to driving depends on how well the heart muscle is pumping.
4.2. Factors Influencing Driving Restrictions
Several factors influence the duration of driving restrictions:
- Type of Procedure: Angiograms and angioplasties have different recovery periods.
- Heart Muscle Function: After a heart attack, the extent of damage to the heart muscle affects driving eligibility.
- Overall Health: Your general health and any other medical conditions can influence the decision.
4.3. Group 2 Licence Holders (LGV / PCV)
If you hold a group 2 licence (LGV / PCV), which allows you to drive large goods vehicles or passenger-carrying vehicles, you have additional requirements:
- Inform the DVLA: You must inform the DVLA of your condition.
- Driving Restrictions: You are not able to drive this type of vehicle for at least 6 weeks.
- Additional Tests: You may need additional tests to fulfill the DVLA requirements for a group 2 licence.
4.4. Safety Tips for Driving
Once you are cleared to drive, follow these safety tips:
- Plan Your Route: Choose routes that are familiar and less stressful.
- Avoid Peak Hours: Drive during off-peak hours to minimize traffic congestion.
- Take Breaks: Stop for regular breaks to rest and stretch.
- Monitor Symptoms: Be aware of any symptoms such as chest pain, dizziness, or shortness of breath.
- Carry Medications: Keep your medications readily accessible in case you need them.
4.5. When to Seek Medical Advice
Seek immediate medical advice if you experience any of the following while driving:
- Chest Pain: Any new or worsening chest pain.
- Dizziness or Lightheadedness: Feeling faint or lightheaded.
- Shortness of Breath: Difficulty breathing.
- Palpitations: Irregular or rapid heartbeats.
5. Returning to Work After Angiogram: A Gradual Approach
How soon can you return to work after an angiogram, and what factors should you consider? The timing of your return to work depends on the nature of your job and the type of procedure you underwent. Generally, you can return to work three days after an angiogram and one week after an angioplasty. If you have had a heart attack, you will likely need four to six weeks off work.
5.1. General Guidelines for Returning to Work
The following are general guidelines for returning to work after cardiac procedures:
- After an Angiogram: 3 days.
- After an Angioplasty: 1 week.
- After a Heart Attack: 4 to 6 weeks.
5.2. Factors Influencing Return to Work
Several factors influence when you can return to work:
- Type of Procedure: Angiograms and angioplasties have different recovery periods.
- Nature of Your Job: Physical demands, stress levels, and working environment all play a role.
- Overall Health: Your general health and any other medical conditions can influence the decision.
5.3. Assessing Your Job’s Physical Demands
Consider the physical demands of your job:
- Sedentary Jobs: If your job is mostly sedentary, you may be able to return sooner.
- Physically Demanding Jobs: If your job involves heavy lifting, strenuous activity, or prolonged standing, you may need more time to recover.
5.4. Managing Stress in the Workplace
Stress can strain your heart, so it’s important to manage stress in the workplace:
- Identify Stressors: Recognize what triggers stress at work.
- Develop Coping Strategies: Use relaxation techniques, time management strategies, and seek support from colleagues or supervisors.
- Take Breaks: Schedule regular breaks to relax and recharge.
5.5. Phased Return to Work
Consider a phased return to work to ease back into your job:
- Start with Reduced Hours: Gradually increase your working hours over several weeks.
- Modify Job Duties: Temporarily modify your job duties to reduce physical or emotional stress.
- Communicate with Your Employer: Keep your employer informed about your progress and any limitations you may have.
5.6. Medical Clearance
Before returning to work, obtain medical clearance from your doctor. They can assess your condition and provide recommendations tailored to your specific needs.
6. The Role of Cardiac Rehabilitation in Recovery
How does cardiac rehabilitation support your recovery after an angiogram or angioplasty? Cardiac rehabilitation is a tailored treatment and prevention program delivered by a team of healthcare professionals. It helps improve the health and wellbeing of people who have heart problems. It is important to take part in Cardiac Rehab as it can support you to improve your heart health.
6.1. What is Cardiac Rehabilitation?
Cardiac rehabilitation is a comprehensive program designed to help individuals recover from heart conditions and procedures. It includes:
- Exercise Training: Supervised exercise sessions to improve cardiovascular fitness.
- Education: Information on heart-healthy lifestyle changes, including diet, smoking cessation, and stress management.
- Counseling: Support to address emotional and psychological challenges.
6.2. Benefits of Cardiac Rehabilitation
Participating in cardiac rehabilitation can provide numerous benefits:
- Improved Cardiovascular Health: Exercise training can strengthen your heart and improve blood flow.
- Reduced Risk of Future Events: Lifestyle changes can lower your risk of heart attacks and other cardiac events.
- Enhanced Quality of Life: Rehabilitation can help you regain your independence and enjoy life more fully.
- Better Medication Adherence: Education can improve your understanding of your medications and the importance of taking them as prescribed.
- Emotional Support: Counseling can help you cope with anxiety, depression, and other emotional challenges.
6.3. Components of Cardiac Rehabilitation Programs
Cardiac rehabilitation programs typically include the following components:
- Medical Evaluation: Assessment of your cardiovascular health and risk factors.
- Exercise Prescription: Customized exercise plan based on your individual needs and abilities.
- Nutritional Counseling: Guidance on heart-healthy eating habits.
- Psychological Support: Counseling to address emotional and psychological issues.
- Education: Information on heart disease, medications, and lifestyle changes.
6.4. Accessing Cardiac Rehabilitation Services
After your angiogram or angioplasty, your nurse will refer you to the community Cardiac Rehabilitation team, who will contact you at home following discharge. These services can be accessed through:
- Hospital-Based Programs: Many hospitals offer cardiac rehabilitation programs.
- Community-Based Programs: Some community centers and clinics also provide cardiac rehabilitation services.
- Online Programs: Telehealth options are increasingly available for those who cannot attend in-person sessions.
6.5. Making the Most of Cardiac Rehabilitation
To maximize the benefits of cardiac rehabilitation:
- Attend Regularly: Consistent attendance is essential for achieving results.
- Follow the Exercise Plan: Adhere to the exercise plan prescribed by your healthcare team.
- Ask Questions: Don’t hesitate to ask questions about your condition, medications, or lifestyle changes.
- Participate Actively: Engage actively in all aspects of the program.
- Seek Support: Connect with other participants and share your experiences.
7. Medication Management Post-Angiogram: A Crucial Aspect
Why is medication management crucial after an angiogram or angioplasty, and how should you manage your medications effectively? Proper medication management is essential to prevent complications and maintain your heart health. After an angioplasty, there is a small risk of problems developing within the treated area, so it is important to take 2 types of tablet to reduce the stickiness of the blood.
7.1. Understanding Prescribed Medications
Before leaving the hospital, your healthcare team will explain your medications to you. Common medications prescribed after an angiogram or angioplasty include:
- Antiplatelet Medications: Such as aspirin, clopidogrel, or ticagrelor, to prevent blood clots.
- Anticoagulant Medications: Such as warfarin, apixaban, rivaroxaban, dabigatran, or edoxaban, especially if you have atrial fibrillation or other conditions that increase the risk of blood clots.
- Statins: To lower cholesterol levels and reduce the risk of plaque buildup in your arteries.
- Beta-Blockers: To slow your heart rate and lower blood pressure.
- ACE Inhibitors or ARBs: To lower blood pressure and protect your kidneys.
7.2. Adhering to Medication Regimen
Adhering to your medication regimen is critical for preventing complications:
- Take Medications as Prescribed: Follow the instructions provided by your healthcare provider.
- Do Not Skip Doses: Take your medications at the same time each day to maintain consistent blood levels.
- Use a Pill Organizer: A pill organizer can help you keep track of your medications.
- Set Reminders: Use alarms or reminders to ensure you don’t miss a dose.
7.3. Potential Side Effects
Be aware of potential side effects of your medications:
- Antiplatelet Medications: Increased risk of bleeding, bruising, or stomach upset.
- Anticoagulant Medications: Increased risk of bleeding, requiring regular blood tests to monitor blood clotting.
- Statins: Muscle pain, liver problems, or digestive issues.
- Beta-Blockers: Fatigue, dizziness, or slow heart rate.
- ACE Inhibitors or ARBs: Cough, dizziness, or kidney problems.
7.4. Managing Side Effects
If you experience side effects, do not stop taking your medications without consulting your healthcare provider. They may be able to adjust your dose or recommend alternative medications.
7.5. Interactions with Other Medications
Be aware of potential interactions between your heart medications and other medications, including over-the-counter drugs, supplements, and herbal remedies. Inform your healthcare provider of all medications you are taking.
7.6. When to Seek Medical Advice
Seek immediate medical advice if you experience any of the following:
- Severe Bleeding: Such as nosebleeds, heavy menstrual bleeding, or blood in your stool or urine.
- Allergic Reactions: Such as rash, hives, swelling, or difficulty breathing.
- Chest Pain: Any new or worsening chest pain.
- Dizziness or Lightheadedness: Feeling faint or lightheaded.
- Shortness of Breath: Difficulty breathing.
8. Lifestyle Changes for Long-Term Heart Health
What lifestyle changes can you make to improve your heart health and reduce the risk of future cardiac events? Making lifestyle changes is crucial for long-term heart health. By adopting a heart-healthy lifestyle, you can reduce your risk of future cardiac events and improve your overall wellbeing. The British Heart Foundation produces a number of patient leaflets which can be ordered from them or downloaded from their website: www.bhf.org.uk.
8.1. Heart-Healthy Diet
Follow a heart-healthy diet that is low in saturated and trans fats, cholesterol, and sodium:
- Eat Plenty of Fruits and Vegetables: Aim for at least five servings per day.
- Choose Whole Grains: Opt for whole grains over refined grains.
- Select Lean Protein Sources: Choose lean meats, poultry without skin, fish, beans, and lentils.
- Limit Saturated and Trans Fats: Avoid fried foods, processed snacks, and fatty meats.
- Reduce Sodium Intake: Limit processed foods and use salt sparingly.
8.2. Regular Exercise
Engage in regular physical activity:
- Aim for at least 150 minutes of moderate-intensity exercise per week.
- Choose activities you enjoy: Such as walking, cycling, swimming, or dancing.
- Start Slowly: Gradually increase the intensity and duration of your workouts.
8.3. Quit Smoking
If you smoke, quit:
- Smoking damages your heart and blood vessels and increases your risk of heart disease.
- Seek support from your healthcare provider or a smoking cessation program.
8.4. Manage Stress
Manage stress through relaxation techniques:
- Practice Relaxation Techniques: Such as deep breathing, meditation, or yoga.
- Get Enough Sleep: Aim for 7-8 hours of sleep per night.
- Connect with Others: Spend time with family and friends.
- Engage in Hobbies: Pursue activities you enjoy.
8.5. Maintain a Healthy Weight
Maintain a healthy weight:
- Being overweight or obese increases your risk of heart disease.
- Work with your healthcare provider to develop a weight management plan.
8.6. Limit Alcohol Consumption
Limit alcohol consumption:
- Excessive alcohol intake can raise blood pressure and increase your risk of heart disease.
- If you drink alcohol, do so in moderation (no more than one drink per day for women and two drinks per day for men).
9. Understanding Potential Complications
What are the potential complications after an angiogram or angioplasty, and how can you recognize and manage them? While angiograms and angioplasties are generally safe, potential complications can occur. It’s important to be aware of these complications and know when to seek medical attention.
9.1. Bleeding at the Insertion Site
Bleeding at the insertion site is a common complication:
- Apply Pressure: If bleeding occurs, apply firm pressure to the site for 10-15 minutes.
- Seek Medical Attention: If bleeding does not stop, seek immediate medical attention.
9.2. Infection at the Insertion Site
Infection at the insertion site can occur:
- Monitor for Signs of Infection: Such as increased pain, redness, swelling, pus, or fever.
- Seek Medical Attention: If you suspect an infection, seek medical attention promptly.
9.3. Allergic Reaction to Contrast Dye
Allergic reactions to contrast dye are rare but can be serious:
- Inform Your Healthcare Provider: If you have a history of allergies, inform your healthcare provider before the procedure.
- Monitor for Symptoms: Such as rash, hives, itching, swelling, or difficulty breathing.
- Seek Emergency Care: If you experience severe symptoms, seek emergency medical care.
9.4. Kidney Damage
The contrast dye used in angiograms can sometimes damage the kidneys:
- Stay Hydrated: Drink plenty of fluids before and after the procedure to help flush out the dye.
- Monitor Kidney Function: Your healthcare provider may monitor your kidney function with blood tests.
9.5. Blood Clots
Blood clots can form in the arteries after an angioplasty:
- Take Antiplatelet Medications: As prescribed to prevent blood clots.
- Seek Medical Attention: If you experience chest pain, shortness of breath, or other symptoms of a heart attack.
9.6. Restenosis
Restenosis is the re-narrowing of an artery after angioplasty:
- Monitor for Symptoms: Such as chest pain or shortness of breath.
- Follow-Up Appointments: Attend follow-up appointments to monitor your condition.
10. Support and Resources for Heart Patients
Where can you find support and resources to help you manage your heart health? Numerous support and resources are available to help you manage your heart health and cope with the challenges of heart disease.
10.1. Cardiac Rehabilitation Programs
Cardiac rehabilitation programs provide comprehensive support and education:
- Exercise Training: Supervised exercise sessions to improve cardiovascular fitness.
- Education: Information on heart-healthy lifestyle changes.
- Counseling: Support to address emotional and psychological challenges.
10.2. Support Groups
Support groups offer a safe and supportive environment:
- Connect with Others: Share experiences and learn from others who have heart disease.
- Gain Emotional Support: Receive encouragement and understanding from fellow patients.
- Learn Coping Strategies: Discover effective ways to manage your condition.
10.3. Online Resources
Numerous online resources provide valuable information and support:
- The British Heart Foundation: Offers information on heart disease, lifestyle changes, and support services.
- The American Heart Association: Provides resources on heart health, prevention, and treatment.
- The National Heart, Lung, and Blood Institute: Offers information on heart disease research and education.
10.4. Healthcare Professionals
Healthcare professionals can provide personalized support and guidance:
- Cardiologists: Specialists in the diagnosis and treatment of heart disease.
- Nurses: Provide education and support to patients and their families.
- Dietitians: Offer guidance on heart-healthy eating habits.
- Psychologists: Provide counseling to address emotional and psychological issues.
10.5. Family and Friends
Family and friends can offer valuable support:
- Communicate Openly: Share your feelings and concerns with loved ones.
- Seek Practical Help: Ask for assistance with tasks such as transportation, meal preparation, or household chores.
- Encourage Healthy Habits: Enlist their support in adopting heart-healthy lifestyle changes.
By utilizing these support and resources, you can improve your heart health, cope with the challenges of heart disease, and enhance your overall wellbeing.
11. TRAVELS.EDU.VN: Your Partner in Post-Angiogram Travel Planning
How can TRAVELS.EDU.VN help you plan safe and enjoyable travel after an angiogram? TRAVELS.EDU.VN understands the unique concerns of travelers who have recently undergone medical procedures. We offer personalized travel planning services to ensure your trip is safe, comfortable, and stress-free.
11.1. Personalized Travel Consultations
TRAVELS.EDU.VN provides personalized travel consultations to assess your individual needs and concerns:
- Medical History Review: We take into account your medical history, including your angiogram and any other medical conditions.
- Doctor Consultation: We encourage you to consult with your doctor before making any travel plans.
- Risk Assessment: We assess potential risks and complications associated with your travel plans.
11.2. Customized Travel Itineraries
We create customized travel itineraries tailored to your specific requirements:
- Accommodation: We select accommodations that are comfortable and accessible.
- Transportation: We arrange transportation that minimizes physical strain and stress.
- Activities: We recommend activities that are appropriate for your fitness level.
11.3. Medical Support Services
TRAVELS.EDU.VN can arrange medical support services to ensure your safety and wellbeing:
- Medical Escorts: We can provide medical escorts to accompany you on your trip.
- Medical Facilities: We identify medical facilities along your route in case of emergencies.
- Emergency Assistance: We provide 24/7 emergency assistance to address any medical issues that may arise.
11.4. Travel Insurance Assistance
We assist you in obtaining appropriate travel insurance:
- Policy Review: We review travel insurance policies to ensure they cover your medical needs.
- Coverage Options: We help you select the right coverage options for your specific situation.
- Claims Assistance: We provide assistance with filing insurance claims if necessary.
11.5. Contact Us
Ready to plan your post-angiogram trip with confidence? Contact TRAVELS.EDU.VN today:
- Address: 123 Main St, Napa, CA 94559, United States
- WhatsApp: +1 (707) 257-5400
- Website: TRAVELS.EDU.VN
Let TRAVELS.EDU.VN take the stress out of travel planning so you can focus on enjoying your trip.
12. Napa Valley: A Perfect Destination for Post-Angiogram Travel
Why is Napa Valley an ideal destination for travelers recovering from an angiogram? Napa Valley offers a serene and relaxing environment, perfect for those seeking a rejuvenating getaway after a medical procedure. With its picturesque vineyards, world-class wineries, and gourmet dining experiences, Napa Valley provides a tranquil escape.
12.1. Relaxing Activities
Napa Valley offers a variety of relaxing activities:
- Wine Tasting: Enjoy leisurely wine tastings at renowned wineries.
- Scenic Drives: Take scenic drives through the rolling hills and vineyards.
- Spa Treatments: Indulge in spa treatments at luxurious resorts.
- Hot Air Balloon Rides: Experience breathtaking views of the valley from above.
12.2. Comfortable Accommodations
Napa Valley boasts a range of comfortable accommodations:
- Luxury Resorts: Stay at upscale resorts with amenities such as spas, pools, and fine dining restaurants.
- Boutique Hotels: Choose from charming boutique hotels with personalized service.
- Bed and Breakfasts: Enjoy cozy and intimate bed and breakfast inns.
12.3. Gourmet Dining
Napa Valley is a food lover’s paradise:
- Michelin-Starred Restaurants: Dine at world-class restaurants with Michelin stars.
- Farm-to-Table Cuisine: Savor fresh, locally sourced ingredients.
- Wine Pairings: Experience exquisite wine pairings with your meals.
12.4. Easy Accessibility
Napa Valley is easily accessible:
- San Francisco International Airport (SFO): Fly into SFO and take a scenic drive to Napa Valley.
- Oakland International Airport (OAK): Alternatively, fly into OAK, which is also within driving distance of Napa Valley.
- Ground Transportation: Rent a car, hire a private driver, or take a shuttle to explore the valley.
12.5. Medical Facilities
Napa Valley has access to quality medical facilities:
- Queen of the Valley Medical Center: Provides comprehensive medical care.
- Local Clinics: Offers a range of medical services.
12.6. Plan Your Napa Valley Getaway with TRAVELS.EDU.VN
Let TRAVELS.EDU.VN help you plan your perfect post-angiogram getaway to Napa Valley:
- Customized Itineraries: We create itineraries tailored to your specific needs and preferences.
- Accommodation Arrangements: We book comfortable and accessible accommodations.
- Transportation Assistance: We arrange transportation to and from Napa Valley.
- Activity Recommendations: We suggest relaxing and enjoyable activities.
Contact TRAVELS.EDU.VN today to start planning your rejuvenating trip to Napa Valley.
13. Addressing Your Concerns: FAQs About Post-Angiogram Travel
Do you have questions about traveling after an angiogram? Here are answers to some frequently asked questions to ease your concerns:
13.1. How Long Should I Wait to Travel After an Angiogram?
Generally, it’s safe to travel after two days following an angiogram or routine angioplasty. However, consult your doctor for personalized advice.
13.2. Can I Fly After Angioplasty with Stent Placement?
Yes, you can fly after angioplasty with stent placement, but wait at least two days and consult your doctor.
13.3. What Precautions Should I Take During Air Travel?
Stay hydrated, move around regularly, wear compression stockings, and avoid alcohol and caffeine.
13.4. Is It Safe to Drive After an Angiogram?
Do not drive for three days after an angiogram and one week after a planned angioplasty.
13.5. When Can I Return to Work After Angioplasty?
You can generally return to work after one week following an angioplasty, depending on your job’s physical demands.
13.6. What Medications Will I Need After Angioplasty?
You will likely need antiplatelet medications such as aspirin and clopidogrel, as well as other medications to manage your heart condition.
13.7. How Does Cardiac Rehabilitation Help After Angioplasty?
Cardiac rehabilitation improves cardiovascular health, reduces the risk of future events, and enhances your quality of life.
13.8. What Lifestyle Changes Should I Make After Angioplasty?
Adopt a heart-healthy diet, exercise regularly, quit smoking, manage stress, and maintain a healthy weight.
13.9. What Are the Potential Complications After Angioplasty?
Potential complications include bleeding, infection, allergic reactions, kidney damage, blood clots, and restenosis.
13.10. How Can TRAVELS.EDU.VN Help Me Plan My Post-Angioplasty Travel?
travels.edu.vn offers personalized travel consultations, customized itineraries, medical support services, and travel insurance assistance to ensure your trip is safe and comfortable.
14. Securing Your Health While Traveling: Insurance and Medical Assistance
Why is it important to have travel insurance and know how to access medical assistance when traveling after an angiogram? Having adequate travel insurance and knowing how to access medical assistance can provide peace of mind and protect you from unexpected medical expenses.
14.1. Importance of Travel Insurance
Travel insurance is essential for covering medical expenses:
- Medical Emergencies: Provides coverage for unexpected medical emergencies.
- Trip Cancellations: Reimburses you for trip cancellations due to medical reasons.
- Lost or Stolen Items: Covers the cost of lost or stolen items.
14.2. Types of Travel Insurance
There are different types of travel insurance policies:
- Comprehensive Policies: Cover medical expenses, trip cancellations, lost items, and other potential issues.
- Medical-Only Policies: Focus solely on medical expenses.
- Trip Cancellation Policies: Cover trip cancellations due to medical or other reasons.
14.3. What to Look for in a Travel Insurance Policy
When selecting a travel insurance policy, consider the following:
- Coverage Limits: Ensure the policy provides adequate coverage for medical expenses.
- Pre-Existing Conditions: Check if the policy covers pre-existing medical conditions.
- Exclusions: Be aware of any exclusions in the policy.
- Emergency Assistance: Ensure the policy provides 24/7 emergency assistance.
14.4. How to Access Medical Assistance
Know how to access medical assistance while traveling:
- Emergency Contacts: Keep a list of emergency contacts with you.
- Local Medical Facilities: Identify local medical facilities in advance.
- Insurance Provider: Contact your insurance provider for assistance.
14.5. Medical Information
Carry essential medical information:
- Medical History: Bring a summary of your medical history.
- Medication List: Keep a list of your medications with dosages.
- Allergies: Note any allergies you have.
