Coughs, those forceful expulsions of air, are a common occurrence, but How Far Do Coughs Travel? Generally, coughs can propel droplets containing respiratory pathogens a considerable distance, impacting transmission of infections like the flu and COVID-19. At TRAVELS.EDU.VN, we’re dedicated to providing you with the most current information and practical guidance to help you stay safe. This article delves into the science behind droplet spread, exploring factors that influence how far coughs travel and effective prevention strategies. Stay informed with TRAVELS.EDU.VN for all your travel health insights, including risk mitigation, infectious disease transmission, and respiratory hygiene.
1. What Factors Influence How Far Coughs Travel?
The distance a cough travels depends on a combination of elements that start with the physics of the cough itself, and continue to environmental conditions, and even the characteristics of the particles expelled.
- Force of the Cough: A more forceful cough expels droplets at a higher velocity, naturally leading to a greater travel distance. Think of it as throwing a ball; the harder you throw, the further it goes.
- Droplet Size: Larger droplets are heavier and more affected by gravity, causing them to fall to the ground quicker. Smaller droplets, conversely, can remain suspended in the air for longer periods and travel greater distances.
- Environmental Conditions: Humidity, temperature, and airflow all play roles. Higher humidity can cause droplets to grow in size as they absorb moisture, making them fall faster. Air currents can carry smaller droplets even further.
- Clothing and Obstacles: Clothes can affect the path of coughs and sneezes as can anything that might block coughs or sneezes.
- Individual Physiology: People are different so the same cough or sneeze from two different individuals could result in different outcomes.
2. What Is the 6-Foot Rule, and How Effective Is It?
For a while the recommendation was to stay 6 feet away from people who are sick to avoid getting sick.
The “6-foot rule” suggests maintaining a distance of at least 6 feet (approximately 2 meters) from others to reduce the risk of respiratory droplet transmission. Research suggests that larger respiratory droplets containing pathogens like influenza can travel approximately 6 feet when a sick person coughs or sneezes.
However, it’s not a foolproof solution. The effectiveness of the 6-foot rule depends on the factors mentioned above, and some studies indicate that droplets can travel beyond this distance, especially in enclosed spaces with poor ventilation. Smaller particles can travel more than 8 feet horizontally through the air. Also, smaller droplets could spray 13–20 feet vertically in the air.
 Person coughing in public, emphasizing the need for awareness and precautions against droplet spread.
Person coughing in public, emphasizing the need for awareness and precautions against droplet spread.
3. How Does Ventilation Affect Droplet Travel Distance?
Ventilation plays a critical role in diluting and removing airborne droplets, thereby reducing the risk of infection. Good ventilation systems introduce fresh air, which dilutes the concentration of droplets containing viruses or bacteria. Air changes per hour (ACH) is a key metric; the higher the ACH, the faster contaminated air is replaced with clean air.
According to a study by the University of Hong Kong, proper ventilation can reduce the concentration of airborne particles by up to 80%, significantly decreasing the risk of airborne transmission in indoor settings. Conversely, poorly ventilated spaces allow droplets to linger, increasing the likelihood of inhalation by others. Smaller droplets could spray 13–20 feet vertically in the air, which is theoretically high enough to enter and travel through ceiling ventilation systems in some buildings.
4. What’s the Difference Between Droplet Transmission and Airborne Transmission?
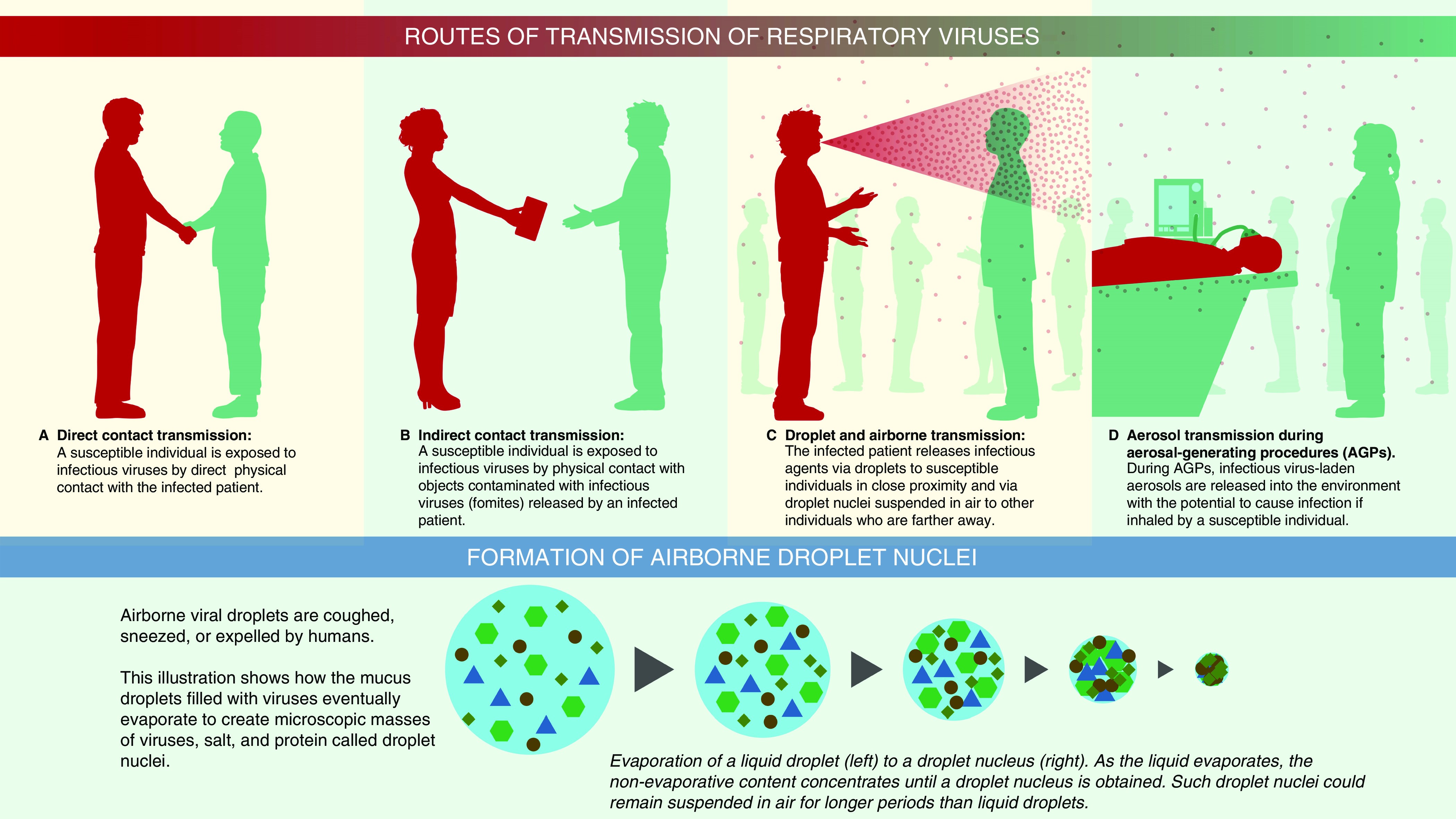
Understanding the difference between droplet and airborne transmission is crucial for implementing effective preventive measures:
| Transmission Type | Droplet Size | Distance Traveled | Suspension Time |
|---|---|---|---|
| Droplet Transmission | Larger (5-10 μm) | Short (up to 6 feet) | Falls quickly |
| Airborne Transmission | Smaller (≤5 μm) | Longer (beyond 6 feet) | Remains suspended |
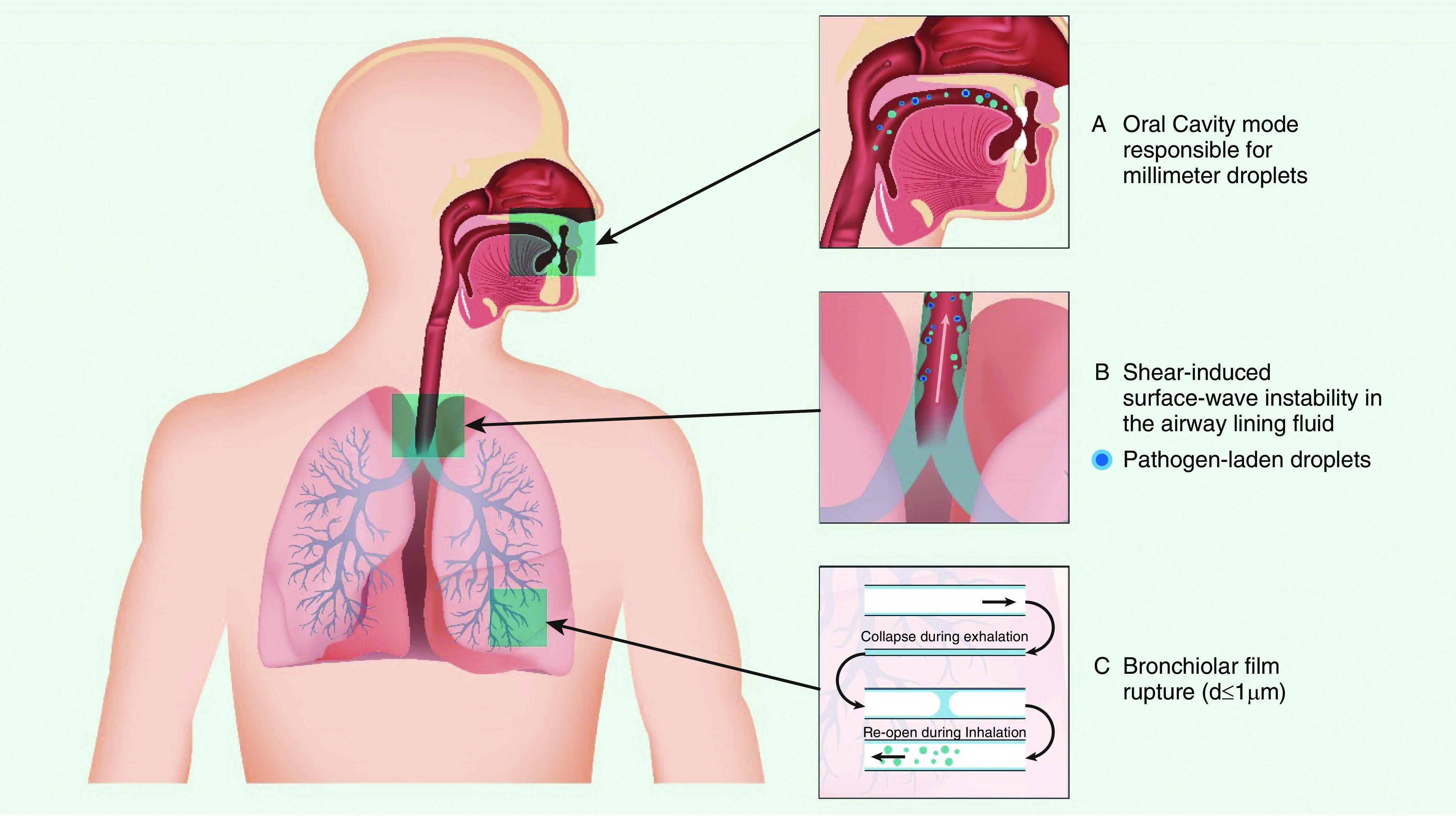
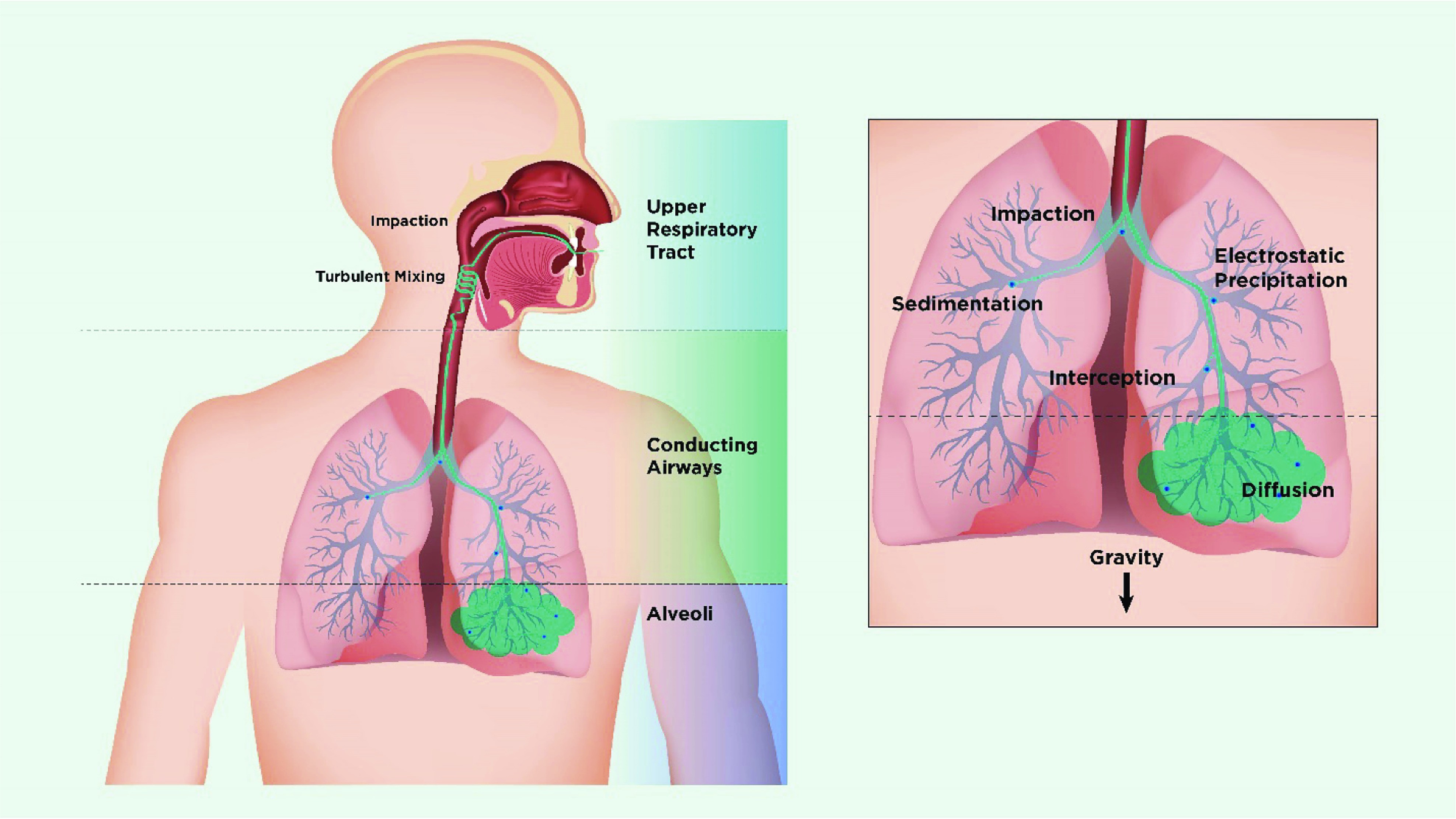
Droplet transmission occurs when larger respiratory droplets are expelled during coughing, sneezing, or talking and come into direct contact with the mucosal surfaces (eyes, nose, mouth) of a susceptible person. These droplets are relatively heavy and fall to the ground within a short distance.
Airborne transmission involves smaller droplet nuclei that can remain suspended in the air for extended periods and travel longer distances. These particles can be inhaled and penetrate deep into the respiratory tract, increasing the risk of infection.
5. Which Respiratory Infections Are Spread Primarily Through Droplets vs. Airborne Transmission?
Different respiratory infections have varying modes of transmission, influencing the effectiveness of different preventive measures:
| Infection | Primary Transmission Mode | Examples of Preventive Measures |
|---|---|---|
| Influenza (Flu) | Droplet | Hand hygiene, social distancing, covering coughs and sneezes |
| COVID-19 | Droplet (primarily) | Mask-wearing, social distancing, hand hygiene, ventilation |
| Measles | Airborne | Vaccination, isolation of infected individuals, ventilation |
| Tuberculosis (TB) | Airborne | Ventilation, respiratory protection (N95 respirators), early detection and treatment |
6. How Effective Are Masks in Preventing Droplet Spread?
Masks are a critical tool in preventing the spread of respiratory infections by blocking the expulsion of droplets and reducing inhalation of airborne particles.
- Surgical Masks: These masks primarily block larger respiratory droplets, reducing the risk of droplet transmission. They are effective in preventing the wearer from spreading infection to others.
- N95 Respirators: N95 respirators provide a tighter seal and filter out a higher percentage of airborne particles, offering greater protection against both droplet and airborne transmission. They are particularly effective in healthcare settings or high-risk environments.
A meta-analysis published in The Lancet found that mask-wearing reduced the risk of respiratory infection by 85%. The effectiveness of masks depends on proper fit, consistent use, and the type of mask used.
 People wearing masks in a crowded area, illustrating the importance of mask-wearing in preventing the spread of respiratory infections.
People wearing masks in a crowded area, illustrating the importance of mask-wearing in preventing the spread of respiratory infections.
7. Does Speaking or Singing Spread Droplets as Far as Coughing?
Yes, speaking and singing can also spread respiratory droplets, although typically not as far as a forceful cough or sneeze. The volume and intensity of speech or singing influence the number and distance of droplets expelled.
- Speaking: Loud speaking can generate thousands of fluid droplets from the oral cavity per second.
- Singing: Singing, especially at high volumes, can produce even more droplets than speaking, increasing the risk of transmission in enclosed spaces.
Research has shown that maintaining a distance of at least 6 feet is advisable when speaking or singing, particularly in poorly ventilated areas.
8. How Long Can Viruses Survive in Droplets on Surfaces?
The survival time of viruses in droplets on surfaces varies depending on the type of virus, the surface material, and environmental conditions.
| Virus | Surface | Survival Time |
|---|---|---|
| SARS-CoV-2 | Copper | Up to 4 hours |
| SARS-CoV-2 | Cardboard | Up to 24 hours |
| SARS-CoV-2 | Plastic/Stainless Steel | 2-3 days |
| Influenza | Non-porous surfaces | 24-48 hours |
These contaminated surfaces can be a potential source of transmission to other individuals who touch the same object or surface and then touch their mouth, nose, or eyes. Regular cleaning and disinfection of frequently touched surfaces are essential to reduce the risk of contact transmission.
9. What Are Aerosol-Generating Procedures (AGPs) and Why Are They Risky?
Aerosol-generating procedures (AGPs) are medical procedures that can produce fine aerosol particles, potentially increasing the risk of airborne transmission of respiratory infections.
- Examples of AGPs: Intubation, bronchoscopy, physiotherapy, and suctioning.
- Risks Associated with AGPs: AGPs can provoke cough and disperse bioaerosols farther away from the patient, increasing the risk of infection among healthcare workers.
Healthcare settings implement stringent infection control measures during AGPs, including the use of N95 respirators, enhanced ventilation, and isolation of patients.
10. What Measures Can Be Taken to Reduce Droplet Spread Indoors?
Several measures can be taken to reduce droplet spread indoors, creating a safer environment for everyone:
- Ventilation: Increase ventilation by opening windows and doors, using air purifiers with HEPA filters, and ensuring HVAC systems are functioning optimally.
- Mask-Wearing: Encourage the use of masks, especially in crowded or poorly ventilated areas.
- Social Distancing: Maintain a distance of at least 6 feet from others whenever possible.
- Hand Hygiene: Practice frequent hand washing with soap and water or use hand sanitizers.
- Surface Disinfection: Regularly clean and disinfect frequently touched surfaces.
- Respiratory Etiquette: Cover coughs and sneezes with a tissue or elbow.
By implementing these measures, we can significantly reduce the spread of respiratory infections and protect ourselves and others.
11. What is the Impact of Humidity on Droplet Transmission?
Humidity levels in indoor environments play a significant role in influencing the behavior and transmission of respiratory droplets. The relationship between humidity and droplet transmission is complex, with varying effects depending on the specific humidity range.
- Low Humidity: In environments with low humidity, respiratory droplets tend to evaporate more quickly. This evaporation reduces the size of the droplets, transforming them into smaller, lighter droplet nuclei. These droplet nuclei can remain suspended in the air for longer periods and travel greater distances, enhancing the potential for airborne transmission.
- High Humidity: Conversely, high humidity levels can cause respiratory droplets to absorb moisture from the air, increasing their size and weight. Larger droplets are more likely to settle quickly onto surfaces, reducing the risk of airborne transmission. However, high humidity can also promote the growth of mold and other microorganisms, which may have other adverse health effects.
- Optimal Humidity: Maintaining an optimal humidity level, generally between 40% and 60%, can help strike a balance. This range helps prevent excessive evaporation of droplets while avoiding conditions that promote microbial growth.
Relative humidity of the indoor environment could alter the particle’s aerodynamic diameter, length of time airborne, and viability. Knight estimated that a 1.5-μm hygroscopic particle increases to 2.0 μm in diameter on passage through the nose and to 4.0 μm in the saturated air of the nasopharynx and the lung.
12. How Do Air Purifiers Help in Reducing Airborne Droplets?
Air purifiers equipped with HEPA (High-Efficiency Particulate Air) filters can effectively remove airborne particles, including respiratory droplets and droplet nuclei, from indoor environments. HEPA filters are designed to capture at least 99.97% of particles that are 0.3 microns in diameter, which includes most viruses and bacteria.
- Mechanism of Action: Air purifiers work by drawing air through a series of filters, including a pre-filter to remove larger particles, a HEPA filter to capture fine particles, and sometimes an activated carbon filter to remove odors and gases.
- Benefits of Using Air Purifiers:
- Reduce the concentration of airborne droplets and droplet nuclei.
- Improve air quality by removing dust, allergens, and other pollutants.
- Supplement ventilation in enclosed spaces.
- Considerations When Choosing an Air Purifier:
- Filter Type: Ensure the purifier has a true HEPA filter.
- Room Size: Select a purifier with a capacity suitable for the size of the room.
- Air Change Rate: Look for a purifier with a high air change rate (ACH).
13. What Role Does UV-C Light Play in Disinfecting Airborne Pathogens?
Ultraviolet-C (UV-C) light is a type of ultraviolet radiation that can be used to disinfect air and surfaces by inactivating viruses, bacteria, and other microorganisms. UV-C light damages the genetic material (DNA or RNA) of these pathogens, preventing them from replicating and causing infection.
- Mechanism of Action: UV-C light is most effective at a wavelength of 254 nanometers. When microorganisms are exposed to UV-C light, the radiation disrupts their cellular processes, leading to their inactivation.
- Applications of UV-C Light:
- Air Disinfection: UV-C lamps can be installed in HVAC systems or used as standalone units to disinfect air in occupied or unoccupied spaces.
- Surface Disinfection: UV-C lamps can be used to disinfect surfaces in healthcare settings, laboratories, and other environments where infection control is critical.
- Safety Precautions:
- UV-C light can be harmful to the skin and eyes, so it should only be used when people are not present in the room.
- Follow manufacturer’s instructions carefully when using UV-C devices.
14. How Does Personal Protective Equipment (PPE) Help in Preventing Droplet Spread?
Personal Protective Equipment (PPE) plays a crucial role in preventing the spread of respiratory infections, especially in healthcare settings and other high-risk environments. PPE includes masks, respirators, gloves, gowns, and eye protection.
- Types of PPE and Their Functions:
- Masks: Surgical masks block larger respiratory droplets, protecting others from the wearer’s respiratory secretions.
- Respirators: N95 respirators provide a tighter seal and filter out a higher percentage of airborne particles, protecting the wearer from inhaling infectious aerosols.
- Gloves: Gloves prevent the transfer of pathogens from contaminated surfaces to the hands.
- Gowns: Gowns protect clothing and skin from contamination with respiratory secretions or other bodily fluids.
- Eye Protection: Face shields or goggles protect the eyes from exposure to respiratory droplets.
- Proper Use of PPE:
- Ensure PPE fits properly and is worn correctly.
- Follow proper donning and doffing procedures to avoid self-contamination.
- Dispose of used PPE safely and appropriately.
15. What Role Do Vaccinations Play in Reducing Droplet Transmission?
Vaccinations are a highly effective tool in reducing the spread of respiratory infections by preventing or reducing the severity of illness. When a large proportion of the population is vaccinated, it creates herd immunity, which protects unvaccinated individuals by reducing the overall transmission of the disease.
- How Vaccinations Work:
- Vaccines stimulate the immune system to produce antibodies that recognize and neutralize specific pathogens.
- If a vaccinated person is exposed to the pathogen, their immune system can quickly mount a defense, preventing or reducing the severity of the infection.
- Benefits of Vaccination:
- Reduce the risk of infection and severe illness.
- Decrease the duration and intensity of symptoms.
- Lower the likelihood of transmission to others.
- Examples of Vaccines for Respiratory Infections:
- Influenza vaccine
- COVID-19 vaccine
- Measles, mumps, and rubella (MMR) vaccine
- Pertussis (whooping cough) vaccine
16. How Can Businesses and Public Spaces Minimize Droplet Spread?
Businesses and public spaces can implement a range of measures to minimize droplet spread and create a safer environment for employees and visitors.
- Ventilation:
- Improve ventilation by opening windows and doors.
- Upgrade HVAC systems with HEPA filters.
- Use portable air purifiers with HEPA filters.
- Hygiene Practices:
- Provide hand sanitizing stations.
- Implement regular cleaning and disinfection protocols.
- Encourage frequent hand washing.
- Social Distancing:
- Maintain physical distancing guidelines.
- Use signage to remind people to stay 6 feet apart.
- Limit the number of people in enclosed spaces.
- Mask-Wearing:
- Require or encourage mask-wearing.
- Provide masks for those who need them.
- Employee Health and Safety:
- Implement employee health screening protocols.
- Encourage employees to stay home if they are sick.
- Provide training on infection control practices.
- Signage and Communication:
- Post signs with reminders about hand hygiene, mask-wearing, and social distancing.
- Communicate regularly with employees and visitors about safety measures.
 A well-ventilated office space with employees maintaining social distance and practicing good hygiene.
A well-ventilated office space with employees maintaining social distance and practicing good hygiene.
17. What Are the Latest Recommendations from Health Organizations Regarding Droplet Spread?
Health organizations such as the World Health Organization (WHO) and the Centers for Disease Control and Prevention (CDC) provide updated recommendations on droplet spread and preventive measures.
- Key Recommendations:
- Mask-Wearing: Wear masks in indoor public spaces, especially in areas with high transmission rates.
- Social Distancing: Maintain a distance of at least 6 feet from others.
- Hand Hygiene: Practice frequent hand washing with soap and water or use hand sanitizers.
- Ventilation: Improve ventilation in indoor environments.
- Vaccination: Get vaccinated against respiratory infections, such as influenza and COVID-19.
- Testing: Get tested if you have symptoms of a respiratory infection.
- Isolation: Stay home if you are sick to prevent spreading the infection to others.
- Stay Informed:
- Follow the latest guidelines from health organizations.
- Stay updated on emerging variants and transmission dynamics.
- Adjust preventive measures based on local conditions and risk levels.
18. What is the Role of Personal Responsibility in Minimizing Droplet Spread?
Personal responsibility plays a crucial role in minimizing droplet spread and protecting the health of ourselves and others. Each individual can take actions to reduce the risk of transmission and contribute to a safer environment.
- Key Aspects of Personal Responsibility:
- Mask-Wearing: Wear a mask when in public indoor spaces, especially if you are feeling unwell.
- Hand Hygiene: Wash your hands frequently with soap and water or use hand sanitizer.
- Social Distancing: Maintain physical distance from others, especially in crowded settings.
- Respiratory Etiquette: Cover your coughs and sneezes with a tissue or your elbow.
- Staying Home When Sick: If you feel unwell, stay home to avoid spreading illness to others.
- Vaccination: Get vaccinated against respiratory infections to protect yourself and others.
- Informed Decision-Making: Stay informed about the latest health recommendations and make responsible choices based on the information available.
19. How Does Airflow in Different Environments Impact Droplet Movement?
Airflow patterns in various environments play a significant role in influencing the movement and dispersion of respiratory droplets. Understanding these patterns can help in implementing effective strategies to minimize droplet spread.
- Indoor Environments:
- Ventilation Systems: HVAC systems can create airflow patterns that either dilute or concentrate airborne droplets. Proper maintenance and filtration are essential.
- Natural Ventilation: Opening windows and doors can create cross-ventilation, which helps remove contaminated air.
- Room Layout: Furniture and other objects can affect airflow patterns, creating areas of stagnant air where droplets may accumulate.
- Outdoor Environments:
- Wind: Wind can carry droplets over longer distances, especially in open areas.
- Building Structures: Buildings can create wind tunnels or block airflow, affecting droplet movement in surrounding areas.
- Healthcare Settings:
- Isolation Rooms: Negative pressure rooms are designed to prevent airborne particles from escaping into other areas of the hospital.
- Operating Rooms: Laminar airflow systems can create a unidirectional flow of air, minimizing the risk of contamination.
- Strategies to Manage Airflow:
- Optimize ventilation systems.
- Use air purifiers with HEPA filters.
- Arrange furniture to promote airflow.
- Consider the impact of wind and building structures on outdoor droplet movement.
20. What Emerging Technologies Are Being Developed to Combat Droplet Transmission?
Researchers and engineers are continually developing new technologies to combat droplet transmission and improve infection control.
- Advanced Filtration Systems:
- Enhanced HEPA Filters: Filters with improved efficiency and durability.
- Nanomaterial Filters: Filters that use nanomaterials to capture even smaller particles.
- UV-C Light Innovations:
- Far-UV-C Lighting: UV-C light that is safe for use in occupied spaces.
- Mobile UV-C Disinfection Robots: Robots that use UV-C light to disinfect surfaces and air.
- Air Monitoring Systems:
- Real-Time Air Quality Sensors: Sensors that monitor the concentration of airborne particles and pathogens.
- Smart Ventilation Systems: Systems that adjust ventilation based on real-time air quality data.
- Personal Protective Equipment (PPE) Innovations:
- Self-Disinfecting Masks: Masks that kill pathogens on contact.
- Transparent Masks: Masks that allow for better communication.
- Surface Coatings:
- Antimicrobial Coatings: Coatings that kill pathogens on surfaces.
- Self-Cleaning Surfaces: Surfaces that repel dirt and microorganisms.
These emerging technologies hold promise for improving infection control and reducing the spread of respiratory infections in various settings.
Staying informed about droplet spread is crucial for protecting ourselves and our communities. At TRAVELS.EDU.VN, we’re committed to providing you with the latest information and practical guidance. Remember to practice good hygiene, wear a mask, and stay informed about local health recommendations.
Are you planning a trip to Napa Valley and want to ensure a safe and enjoyable experience? Let TRAVELS.EDU.VN take care of all the details! Our expert travel advisors can help you plan a personalized itinerary, book accommodations, and arrange transportation while ensuring your safety and well-being. Contact us today for a free consultation and let us help you create unforgettable memories.
Ready to plan your perfect Napa Valley getaway? Contact TRAVELS.EDU.VN today!
- Address: 123 Main St, Napa, CA 94559, United States
- WhatsApp: +1 (707) 257-5400
- Website: travels.edu.vn
Frequently Asked Questions (FAQ)
1. How far can droplets travel when someone coughs?
Droplets can travel up to 6 feet or more, depending on the force of the cough and environmental factors.
2. Are masks effective in preventing droplet spread?
Yes, masks, especially N95 respirators, are effective in blocking droplets and reducing the risk of transmission.
3. What is the difference between droplet and airborne transmission?
Droplet transmission involves larger droplets that fall quickly, while airborne transmission involves smaller particles that remain suspended in the air for longer periods.
4. How does ventilation affect droplet travel distance?
Good ventilation dilutes and removes airborne droplets, reducing the risk of infection, while poor ventilation allows droplets to linger.
5. How long can viruses survive in droplets on surfaces?
Survival time varies, but some viruses can last for hours or even days on surfaces like plastic and stainless steel.
6. What are aerosol-generating procedures (AGPs)?
AGPs are medical procedures that can produce fine aerosol particles, increasing the risk of airborne transmission.
7. What measures can be taken to reduce droplet spread indoors?
Increase ventilation, wear masks, practice social distancing, and disinfect surfaces.
8. How does humidity impact droplet transmission?
Low humidity can cause droplets to evaporate and travel further, while high humidity can cause them to settle quickly.
9. Do air purifiers help in reducing airborne droplets?
Yes, air purifiers with HEPA filters can remove airborne particles, including respiratory droplets.
10. What is the role of personal responsibility in minimizing droplet spread?
Each individual should practice good hygiene, wear a mask, and stay home when sick to reduce the risk of transmission.
